Water Balance
- Water is an important solvent of life.
- More important than any other solvent to body.
- Kidney actively participates in metabolism of water.
 Functions/ Role of water:
Functions/ Role of water:
- Provides aqueous medium to the organism which is essential for various biochemical reactions to occur.
- Directly participates as reactant in several metabolic reactions.
- Serves as a vehicle for transport of various solutes.
- Closely associated with regulation of body temperature.
Distribution of water:
- Adult human body contains about 60% water.
- Men 55-70%
- Women 45-60%
Women & Obese individuals: Relatively less water due to higher content of stored fat in anhydrous form.
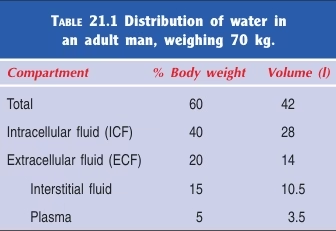 Fig: Distribution of water in the body
Fig: Distribution of water in the body
Water Intake:
Exogenous Water: 0.5 – 5 litres. (Average 2200 ml/day)
- Ingested water & beverages, Solid foods.
- Depends on social habits & climate.
- Controlled by a thirst centre located in the hypothalamus.
Endogenous Water: 300-350 ml
- Metabolic water produced in the body.
- 1000 Cals consumed: 125 ml water.
Water Output
- Urine: 1-2 Ltr/day. (Average 1500 ml/day)
- Major route: controlled by ADH (posterior pituitary hormone).
- ↑ Plasma osmolality: promotes ADH secretion: ↑ Water Re-absorption from renal tubules: Less Urine Output.
- Plasma osmolality depends on sodium concentration, hence Sodium indirectly controls amount of water in the body.
- Diabetes Insipidus: Deficiency of ADH, Increased loss of water.
- Minimum Excretory Volume: 500 ml/day.
- Insensible Water Loss: Perspiration & Respiration.
- Skin: Perspiration- 450 ml/day.
- Depends on atmospheric temp & humidity.
- Fever: increases water loss.
- Lungs: Respiration- 400 ml/day
- Hot climates & Fever: increases water loss.
- Feces: GI tract-150 ml/day
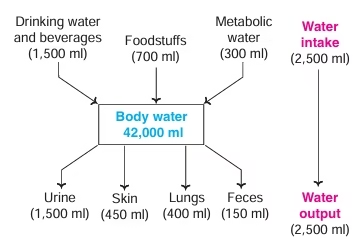 Fig: Water Balance in humans
Fig: Water Balance in humans
Electrolytes Distribution
- Electrolytes are well distributed in body fluids to maintain osmotic equilibrium and water balance. Na+ is the principal cation of ECF, while K+ is the chief cation of ICF.
- Osmolarity: Osmotic pressure exerted by the number of moles per litre of solution.
- Osmolality: Osmotic pressure exerted by the number of moles per kg of solvent.
- Osmolality is more commonly used than osmolarity in clinical practice.
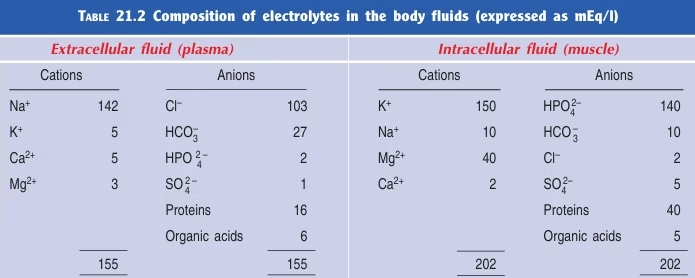 Table: Composition of electrolytes in body compartments (mEq/L)
Table: Composition of electrolytes in body compartments (mEq/L)
Regulation of Water & Electrolyte Balance
- Kidneys
- Hormones : Aldosterone, ADH, Renin-Angiotensin
- ANP
- Kinins : Bradykinin & Kallidin
Aldosterone:
- Mineralo-corticoid produced by adrenal cortex.
- Increases Na + re-absorption;
- At the expense of K+ and H + ions.
ADH (Antidiuretic Hormone)
- Increase in plasma osmolality stimulates hypothalamus to release ADH.
- Increases water Reabsorption.
- Proportionate amounts of sodium and water are retained to maintain the osmolality.
Renin- Angiotensin- Aldosterone System:
- Secretion of Aldosterone is controlled by R-A system.
- Factors stimulating the release of renin include: a) decrease blood volume b) salt depletion c) prostaglandins.
- Factors that inhibit the release of renin are: a) increased blood pressure b) high salt intake c) prostaglandin inhibitors d) Angiotensin II
- Decrease in BP (fall in ECF volume) → Renin (juxtaglomerular apparatus of Nephrons) → Angiotensinogen → Angiotensin I → Angiotensin II → Aldosterone.
- Interrelationship between renin, Angiotensin and Aldosterone plays an important role in regulation of Na+ Reabsorption. Aldosterone & ADH coordinate together to maintain normal fluid and electrolyte balance.
ANP:
- Atrial Natriuretic peptide.
- Polypeptide hormone secreted by Right Atrium of Heart.
- In response to increase IVV
- Causes Natriuresis (Increase Na + excretion)
Bradykinin & kallidin:
- Activated when IVV is increased
- Causes Natriuresis & Diuresis
- Action opposite to ADH & Aldosterone.
Regulation of Fluid Intake
Dehydration
- Decreased blood volume and pressure
- Increased blood osmolarity
Thirst mechanisms
- Stimulation of thirst center (in hypothalamus)
- Angiotensin II: produced in response to decreased BP
- ADH: produced in response to increased blood osmolarity
- Hypothalamic osmoreceptors: signal in response to increased ECF osmolarity
- Inhibition of salivation: thirst center sends sympathetic signals to salivary glands
Regulation of Output:
- Only control over water output is through variations in urine volume
- By controlling Na+ reabsorption (changes volume)
- as Na+ is reabsorbed or excreted, water follows it
- By action of ADH (changes concentration of urine)
- ADH secretion (as well as thirst center) stimulated by hypothalamic osmoreceptors in response to dehydration, prolonged fever, diarrohea, vomiting.
- Effects: slows decreased in water volume and increased osmolarity
Dehydration
Dehydration occurs when water intake is inadequate or when losses are excessive. Excessive water loss is usually associated with a simultaneous electrolyte loss.
Causes of dehydration:
Dehydration may occur as a sequel to diarrhea, vomiting, excessive sweating, fluid loss in burns, adrenocortical dysfunction, kidney diseases (e.g. renal insufficiency), and deficiency of ADH (diabetes insipidus).
Features of dehydration
- Dehydration can be mild, moderate, severe.
- Volume of ECF (Ex- plasma) is decreased coinciding with a rise in electrolyte concentration and osmotic pressure.
- Water is drawn from the ICF, as a result the cells are shrunken flat affecting all the cellular activities (Ex. Increased protein breakdown).
- ADH secretion is increased causing more water retention in the body and this adversely affects urine formation.
- The clinical manifestations of severe dehydration include increased pulse rate, low blood pressure, sunken eyeballs, decreased skin turgor, lethargy, confusion and eventually coma.
Treatment of dehydration
- Intake of plenty of water is a simple and effective method of treating dehydration. In persons who cannot ingest it orally, water can be given via a nasogastric tube. If this is not possible, water should be given intravenously (IV) in an isotonic solution, usually as 5% glucose (5% dextrose). If there is associated electrolyte depletion, (dextrose-saline 4% dextrose, 0.18% NaCl) should be given intravenously.
- When sodium depletion alone is the problem, giving intravenous isotonic fluid – normal saline (0.9% NaCl) or plasma expanders or albumin is the first line of management of salt deficit. After restoring the intravascular volume, the underlying cause must be treated.