
Micro and Macronutrients
- Micronutrients are substances required in very small amounts (mg or μg) and that mainly function as co-factors of enzymes (< 0.005% body weight).
- Examples include:
-
-
- Vitamins
- Trace minerals (Fe, Cu, F, Zn, I, Se, Mn, Mo, Cr, Co and B).
-
- Macronutrients are chemical substances that are required in relatively large amounts (> 0.005% body weight).
- Examples include proteins, fats, carbohydrates and minerals (Na, Mg, K, Ca, P, S and Cl).
Vitamins- Definition
- Vitamins may be regarded as organic compounds required in the diet in small amounts to perform specific biological functions for normal maintenance of optimum growth & health of the organism.
- Vitamins are organic substances that are required in small amount in diet for optimum health & Growth. They are usually not synthesized by humans and hence must be obtained through diet. Plants and bacteria synthesize vitamins on their own.
- The degradation of vitamins does not provide energy (non-calorigenic), but they take part in metabolic reactions that release energy from macronutrients.
- Two Forms of Vitamins:
- Precursor/Provitamin
- Dietary form inactive
- Activated in body
- Active form
- Dietary form active
- Not changed in body
Vitamers:
- Chemically similar substances that possess qualitatively similar vitamin activity.
- Retinol, Retinal & Retinoic Acid are vitamers of vitamin A.
- Generally vitamin deficiencies are multiple rather than individual with overlapping symptoms.
Classification of Vitamins
Broadly vitamins are classified as fat soluble and water soluble vitamins.
Fat Soluble Vitamins:
- Dissolve in organic solvents
- Not readily excreted in urine; can cause toxicity
- Absorbed along with fat
- Deficiency with fat malabsorption
- Fat blockers (Orlistat/Xenical)
- Requires protein carrier
- Transported like fat in chylomicrons, VLDL, LDL
- Stored in body (except Vitamin K)
- Fat tissue/liver
- Can cause toxicity
- Vitamin D and A most likely to be toxic
Water Soluble Vitamins:
- Water soluble
- Absorbed in the intestine
- Transported in blood
- No storage site (Exception Vitamin B12 – liver)
- Toxicities are very rare
- Unlike fat soluble vitamins these can be taken in excess quantity
- Deficiency states are very common
- No specific carrier complexes required
- Most of them are cofactors for enzymes
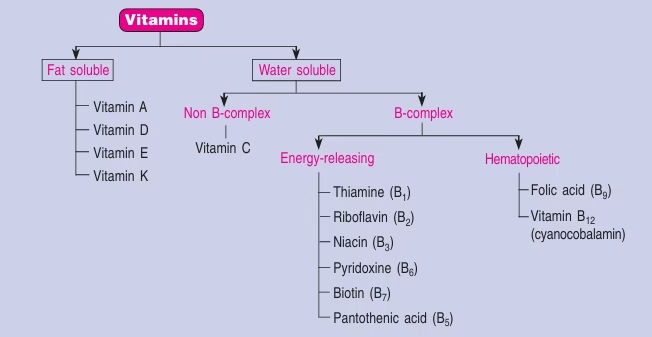 Table: Classification of Vitamins
Table: Classification of Vitamins
Vitamin A
Chemistry:
Retinol, Retinal & Retinoic Acid are vitamers of vitamin A.
- Retinol – Primary alcohol containing β- inone ring.
- Retinal – Aldehyde form obtained by the oxidation of Retinol.
- Retinoic acid – Produced by oxidation of Retinal.
- β-Carotene – Found in plant foods. Cleaved in intestine to produce two moles of Retinal.
Dietary sources:
- Animal Sources : liver, kidney, egg yolk, milk, cheese, butter, fish (cod liver oil)
However, they are generally used as nutritional supplements rather than as food sources.
- Vegetable sources: yellow and dark green vegetables and fruits – carrots, spinach, papaya, pumpkins, mango.
The darker the green leaves, the higher is its carotene content.
Daily requirement (RDA):
1 RE = 1 mg retinol
= 6 mg b-carotene
1 IU = 0.3 mg retinol
The RDA for vitamin A is as follows
Men 1000 RE (3500 IU)
Women 800 RE (2800 IU)
Biochemical Functions:
- Vitamin A is required for dark adaptation in visual cycle.
- Prevents night blindness.
- Prevents xerophthalmia (dry eye).
- Maintains cell health (epithelial cells): maintenance of proper immune system.
- Growth, development, reproduction: retinol & retinoic acid regulate protein synthesis & involved in cell growth & differentiation.
- Cardiovascular disease prevention: carotene prevents heart attacks.
- Cancer (by free radicals &oxidants) prevention as Carotenoids act as
- Retinol & Retinoic acid : Synthesis of Transferrin
- Retinyl phosphate: necessary for synthesis of Glycoproteins are important constituents of mucus. In vitamin A deficiency, lack of mucus secretion results in drying of epithelial tissues.
- Vitamin A is essential for the formation of mucopolysaccharides in the extracellular matrix.
Role in vision:
- Biochemical function of vitamin A in process of vision was first elucidated by George Wald for which he was awarded noble prize in 1968.
- The overall mechanisms through which vitamin A functions in visual system is known as Wald’s visual cycle or Rhodopsin cycle.
Deficiency manifestations:
- Deficiency is most common cause of non-accidental blindness worldwide
- Up to 500,000 children in developing nations especially Asia, become blind each year because of Vitamin A deficiency.
- The clinical signs of vitamin A deficiency mostly involve the eye. Vitamin A deficiency is one of the major causes of preventable blindness.
- Night blindness:
- Night blindness (Nyctalopia) or the inability to see in dim light is the earliest symptom of vitamin A deficiency. It occurs due to impairment of dark adaptation.
- Decrease mucus production leading to bacterial invasion in the eye
- Xerophthalmia: Dryness in conjunctiva & cornea; In conjunctiva- white triangular plaques (Bitot’s spots). Night blindness, if left untreated, causes dryness of the conjunctiva and the cornea. The conjunctiva becomes thick and wrinkled; the cornea loses its mucosal cells and become dull, hazy due to keratinisation and loses its transparency. These changes are described as
- Bitot’s spots
Bitot’s spots are triangular, white patches on the conjunctiva on either side of the cornea. They are usually bilateral.
- Keratomalacia
If the condition progresses beyond xerophthalmia, there is ulceration and necrosis of the cornea (keratomalacia) which results in total blindness. Keratomalacia is one of the major causes of blindness in developing countries and is usually associated with protein energy malnutrition (PEM)
- Irreversible blindness
- Growth retardation
- Sterility in males.
- Vitamin A is essential for the maintenance of the immune system. Its deficiency causes keratinisation of the mucosal lining of the respiratory, gastrointestinal and genitourinary tracts making them susceptible to frequent infections.
- Retinol and retinoic acid are essential for the synthesis of transferrin, the iron transporting protein. Iron deficiency anemia may occur in vitamin A deficiency
Hypervitaminosis A:
Excessive consumption – Symptoms
Dermatitis, enlargement of liver, skeletal decalcification,
Tenderness of long bones, loss of weight, loss of hair, joint pains.
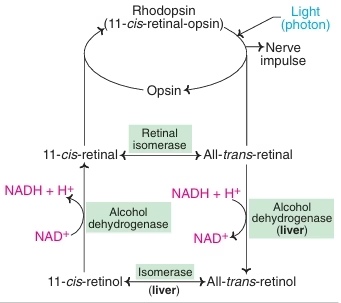 Image: Wald’s Visual Cycle
Image: Wald’s Visual Cycle
Vitamin D
Sources:
- Vitamin D can be derived both from sunlight and food. The human body manufactures vitamin D with the help of sunlight. It also occurs mainly in foods of animal origin.
- Oily fish, egg yolk, liver, butter and cheese contain good quantities. Fish liver oils, although not considered a food, are the richest source of vitamin D. Plant sterol, ergosterol provides a dietary source.
- Breast milk contains relatively small amounts of vitamin D and infants are at risk of developing vitamin D deficiency, particularly premature infants (since the vitamin is transported across the placenta mainly in the last trimester of pregnancy).
Daily requirement (RDA):
- 400 International units or 10 mg cholecalciferol.
- In countries with good sunlight (India), it is 200 IU or 5 mg of cholecalciferol.
Functions:
Vitamin D – precursor is cholesterol, converted by UV from sunlight exposure, therefore is a “non-essential” vitamin.
- Increases calcium absorption in bone, intestines, and kidney. Promotes bone growth and maintenance.
- Stimulates maturation of cells – heart, brain, immune system, etc.
- Synthesis and secretion of parathyroid and thyroid hormones
- Intestine : increases the absorption of calcium and phosphate
- Bones: increases calcium intake in the osteoblasts
- Kidney: decreases the excretion of calcium and phosphate.
- Involved in insulin secretion
Deficiency manifestations:
Rickets: In children
- improper mineralisation
- Bow-legs, knock-knees, pigeon chest, kyphoscoliosis.
- (‘rickety rosary’) (Harrison’s sulcus)
Osteomalacia: In Adults
- Renal rickets
- Vitamin-D resistant rickets
Toxicities (10-100 times RDA)
Loss of calcium from bone and deposition in soft tissues.
Loss of appetite, nausea and vomiting, psychological depression.
.
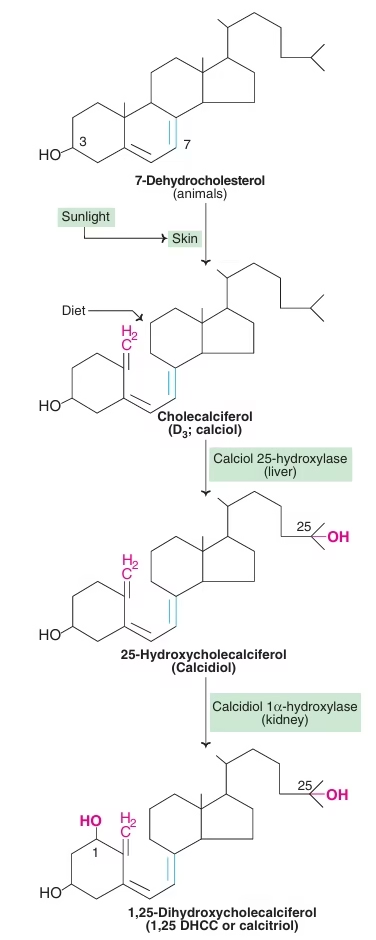 Fig: Formation and activation of vitamin D
Fig: Formation and activation of vitamin D
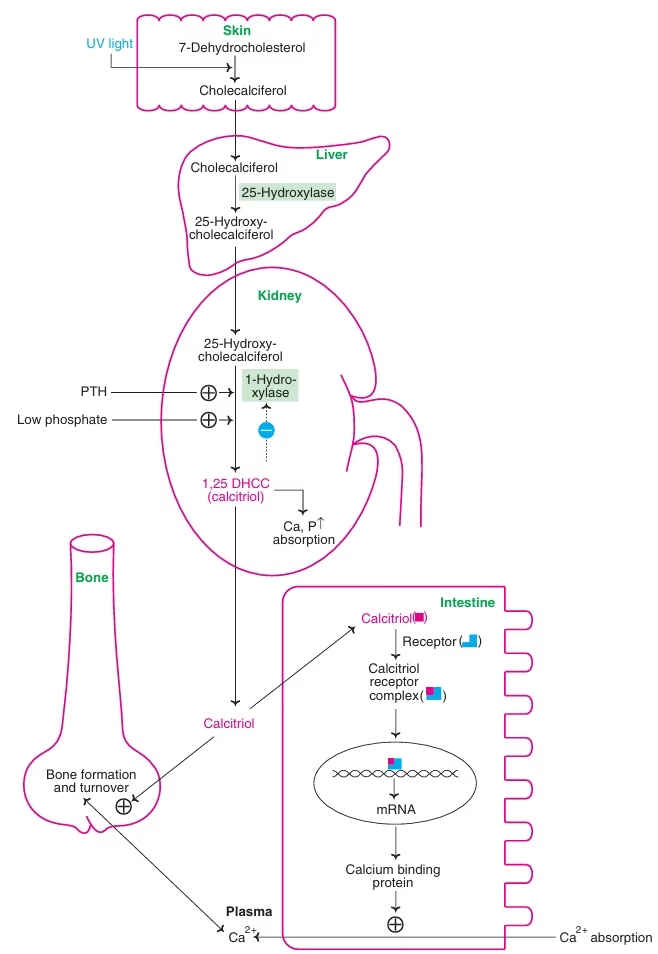 Fig: Biochemical functions of vitamin D
Fig: Biochemical functions of vitamin D
Vitamin C
- Ascorbic acid is a hexose derivative
- Causation factor for (limeys disease ) scurvy
Dietary sources:
- Citrus fruits, gooseberry, guava, green vegetables, tomatoes, potatoes (skin), cabbage.
- Milk is a poor source
Daily requirement (RDA):
60 – 70 mg/day
- Animals can synthesize ascorbic acid by their uronic acid pathway with L-gulonolactone oxidase
Functions:
- Formation of collagen – acts as a coenzyme for the hydroxylation of proline and lysine when procollagen is converted to collagen
- Maintain normal connective tissue & wound healing.
- Bone formation
- Essential in tryptophan, tyrosine, folic acid metabolism
- It is important for maturation of RBCs
- Required for cholesterol metabolism and corticosteroid hormone synthesis
- Enhances iron absorption (ferrous form); Ferritin formation.
- Converts Met-Hb to Hb.
- Degradation of bile pigments requires it.
- Strong Antioxidant property, so sparing action on other vitamins.
- Synthesis of immunoglobulins
- Reuse risk of cancer, cataract & CHD.
Deficiency manifestations:
- Scurvy: Characterized by spongy and sore gums, loose teeth, anemia, swollen joints, fragile blood vessels, decreased immunocompetance, Delayed wound healing.
- Deficiency of vitamin C also results in local haemorrhages and bones become susceptible to fractures. Collagen is also a constituent of the ground substance surrounding capillary walls; hence vitamin C deficiency causes capillary fragility.
Vitamin E
α-Tocopherol is most active
Dietary sources:
Vegetable oils are rich in vitamin E especially wheat germ oil.
Sunflower, safflower, cotton seed oils, corn and soyabean oils are good sources.
Daily requirement (RDA):
10 mg (15 IU)/day (alpha-tocopherol) for men & 8 mg (12 IU) for women
Functions:
- Antioxidant (protects polyunsaturated fats)
- Necessary for normal nerve development
- Essential for membrane structure and integrity of the cell
- Closely associated with reproductive functions and prevents sterility
- Protects liver from toxic compounds CCl4.
- With Vitamin A, Vitamin C & carotene: delay cataract onset
- Prevents oxidation of vitamin A, vitamin C and carotenes
- Required for proper storage of creatine in the skeletal muscle
- For optimum absorption of AAs in intestine
- It reduces cardiovascular complications (reduces LDL oxidation) & Cancer
- Enhances heme production
Deficiency manifestations: Vitamin in search of disease (decreased absorption of fats- liver disease, low fat diets)
- Sterility
- fragile RBCs (hemolysis), anemia
- Loss of muscle coordination, vision, immune functions
Toxicities: Least Toxic (more than 1000 milligrams/day)
- Increases the effects of anticoagulants.
Vitamin K
Chemistry:
Vitamin K exists in different forms,
Vitamin K1 (Phylloquinone) is present in plants,
Vitamin K2 (Menaquinone) is produced by the intestinal bacteria & also found in animals
Vitamin K3 (Menadione) is a synthetic form
Dietary sources:
Green leafy vegetables, cabbage, tomatoes, alfa alfa, spinach, fats and oils, dairy products, animal sources.
Daily requirement (RDA):
- 70-140 μg/day
Strictly there is no RDA for vitamin K, since it can be adequately synthesized in the gut.
Functions:
- A non essential vitamin as its synthesized by the gut bacteria
- Post translation modification of certain clotting factors (factors 2, 7, 9, 10).
- Coenzyme for the carboxylation of glutamic acid residues
- Gamma carboxyglutamate is important in the clotting mechanism
- Carboxylation of Glu residues of osteocalcin.
Deficiency manifestations: Uncommon
- It may occur due to its faulty absorption, loss in feces or administration of antibiotics.
- Blood coagulation is adversely affected.
- Blood clotting time is increased.
- Vitamin K deficiency leads to prolonged coagulation and Newborns, especially preterm infants are more susceptible to vitamin K deficiency.
- Vitamin K deficiency is seen in adults suffering from obstructive jaundice and other diseases causing severe fat malabsorption. Patients suffering from small bowel diseases such as celiac disease, Crohn’s disease suffer from vitamin K deficiency. Patients on long-term antibiotic therapy (antibiotic drugs kill vitamin K synthesising bacteria in the intestine) are also at risk of developing vitamin K deficiency.
Vitamin B1 (Thiamine)
- Anti beriberi or antineuritic vitamin
Dietary sources:
- Whole grain cereals, yeast, legumes, oilseeds and nuts, especially groundnut, are important sources of thiamine. Animal foods such as pork, beef and sheep liver are also good sources.
- Thiamine is mostly concentrated in the outer layer (bran) of cereals. Polishing of rice removes 80% of thiamine.
- It is extracted into water during cooking process. Such water should not be discarded.
- In the parboiled and milled rice, thiamine is not lost in polishing.
Daily requirement (RDA): 1- 1.5mg/day
Functions:
- TPP acts as a coenzyme to three main enzymes-
- Pyruvate dehydrogenase
- α-ketoglutarate dehydrogenase
- Transketolase
- Branched chain α acid dehydrogenase.
- It plays an important role in nerve transmission.
Deficiency manifestations:
Beriberi:
- Seen in populations consuming exclusively polished rice as their staple diet.
- Loss of appetite, vomiting, weakness, mental depression, peripheral neuropathy, irritability, numbness in legs.
Wernicke-Korsakoff syndrome:
- In chronic alcoholics
- Due to insufficient intake or impaired intestinal absorption.
- Loss of memory, apathy, rhythmical to & fro movements of the eyeballs.
Wet beri-beri:
It is characterised by cardiovascular signs and symptoms such as edema of legs, face, trunk and serous cavities.
- Breathlessness & palpitation. Raised SBP.
- Heart weak & death due to Heart Failure.
Dry beri-beri:
In this type, the nervous system is affected. It presents with progressive muscle wasting, peripheral neuropathy of the motor and sensory systems with diminished reflexes.
- Edema not seen. Muscles progressively weaken, walking difficult.
- Symptoms often mixed beri-beri.
Biochemical Changes in Thiamine Deficiency:
- Accumulation of pyruvate: Its increased concentration in plasma & excretion in urine.
- Alteration in Blood Brain Barrier: Pyruvate enters brain, accumulates – polyneuritis.
- Impairment in nerve impulse transmission due to lack of TPP.
- Measurement of RBC transketolase: decreased activity.
Vitamin B2 (Riboflavin)
Coenzymes of Riboflavin
Riboflavin exists in two active coenzyme forms
- Flavin mononucleotide (FMN)
- Flavin adenine dinucleotide (FAD)
- Flavin coenzymes mostly occur as prosthetic groups of oxidoreductase These enzymes are known as flavoproteins.
Dietary sources:
- Milk, milk products, meat, eggs, Liver, kidney
- Moderate sources – cereals, fruits, vegetables, fish.
Daily requirement (RDA): 1.2 – 1.7 mg/day
Functions:
Flavin co-enzymes: Redox reactions.
- Enzymes that utilize flavin coenzymes are called flavoproteins
- Coenzymes often bind rather tightly to the protein either by covalent or noncovalent bonds.
Coenzymes FAD, FMN, are associated with certain enzymes involved in carbohydrate, lipid, protein and purine metabolisms.
Deficiency manifestations:
- Its deficiency usually occurs in association with deficiencies of other B complex vitamins. It usually affects the tongue and lips; characterised by glossitis (magenta tongue), angular stomatitis, cheilosis (fissure-like lesions at the corners of the mouth), pharyngitis and genital dermatitis.
- Laboratory diagnosis done by measurement of FAD-dependent glutathione reductase activity in RBC.
Vitamin B3 (Niacin)
- Pellagra preventive factor of Goldberg
- Nicotinic acid vitamin or Niacin
- Co-factors – NAD, NADP
- Nicotinamide adenine dinucleotide & NAD phosphate.
- It can also be synthesized from tryptophan. 60 mg tryptophan needed: for 1 mg Niacin synthesis.
Dietary sources:
- liver, yeast, whole grains, cereals, pulses, peanuts
- Poor – milk, fish, eggs, vegetables
Daily requirement (RDA): 15 – 20 mg children – 10-15 mg
- One niacin NE = 1mg niacin or 60mg tryptophan
Functions:
The coenzymes NAD & NADP are involved in many oxidation-reduction reactions.
There is a fundamental distinction between NADH and NADPH
- NADH thus generated in various catabolic pathways is oxidised in the respiratory chain to generate ATP. NADH thus plays a vital role in cellular respiration.
- NADPH serves as a readily available reducing power in biological systems. It is used as a reductant in biosynthetic processes.
Deficiency manifestations:
- Pellagra (Italian- rough skin)
- People whose staple diet was corn/maize, jowar (leucine rich) – (vitamin B6 is also required for synthesis)
- Niacin present in maize is unavailable to the body as it is in bound form.
- Symptoms – 4 Ds
- Dermatitis, Diarrhoea, Dementia, Death
- Dermatitis- Inflammation of skin
- Areas exposed to sunlight: neck, dorsal part of feet, ankle & part of the face.
- Diarrhoea: with blood & mucus.
- Dementia: degeneration of nervous tissue. Anxiety, irritability, poor memory, insomnia.
Therapeutic Uses:
- In pharmacological doses 2-4 g/d
- Inhibits lipolysis in adipose tissue.
- TAG synthesis in liver is decreased.
- Treatment of hyperlipoproteinemia type IIb: serum levels of Cholesterol, TG, LDL & HDL lowered.
Vitamin B6 (Pyridoxine)
3 Vitamers – pyridoxine, pyridoxal, pyridoxamine.
- They are Pyridine derivatives.
- Pyridoxamine – plants
- Pyridoxal & Pyridoxamine – animal food.
- Active form of vitamin B6 is coenzyme: Pyridoxal Phosphate (PLP).
Dietary sources:
- Egg yolk, fish, milk & meat are animal sources.
- Wheat, corn, cabbage, roots & tubers are plant sources.
Daily requirement (RDA): 2 to 2.2 mg/day
Functions:
- Protein metabolism
- Involved in reactions such as transamination, decarboxylation, deamination, transsulfuration, etc
Fig: Transamination reaction- Coenzyme PLP
- Involved in formation of haemoglobin (ALA), hormones and structural proteins
- Synthesis of Niacin coenzymes from Tryptophan
- Healthy development of nervous system
- Decarboxylation:
- AAs – Amine ; Decarboxylase
- Serotonin (from Tryptophan): Nerve impulse transmission
- Histamine (from histidine): Vasodilator & lowers the blood pressure
- GABA (from Glutamate): inhibits transmission of nerve impulse.
- Catecholamine (dopamine, NE, E) from tyrosine.
Fig: Decarboxylation reactions: Coenzyme PLP
Deficiency manifestations:
- Neurological:
(Decreased synthesis of serotonin, GABA, NE & E) Tiredness, depression, Fatigue, irritability, peripheral neuropathy, mental confusion
- Infants – convulsions (epilepsy)
- Hypochromic microcytic anemia : reduction in heme production
- Carpal tunnel syndrome
- Hematological manifestations include microcytic, hypochromic anemia due to diminished hemoglobin synthesis. Platelet dysfunction may also occur.
- Dermatological manifestations include seborrheic dermatitis, stomatitis, glossitis and cheilosis.
Drug Interactions:
- Isonicotinic acid hydrazide (INH-isoniazid) inhibits the enzyme pyridoxal kinase, thus affecting the synthesis of PLP adversely.
- Women taking oral contraceptives are prone to develop B6 deficiency as OCP are known to inhibit enzymes dependent on PLP.
- Alcoholism may result in B6 deficiency, as acetaldehyde which is formed from ethanol can compete with PLP for protein binding.
Biotin
- Anti egg white injury factor
- Sulfur containing B complex vitamin.
- Vitamin B7, vitamin H
Dietary sources:
Liver, kidney, egg yolk, milk tomatoes, grains etc.
Daily requirement (RDA): 100 – 300 mg
Functions:
- Serves as a carrier of CO2 in carboxylation reactions catalyzed by pyruvate carboxylase. Pyruvate → oxaloacetate.
- As a coenzyme in Gluconeogenesis, citric acid cycle, Fatty acid synthesis, Metabolism of amino acids.
- Acetyl CoA → Malonyl CoA
- Propionyl CoA → Methyl Malonyl CoA
Deficiency manifestations:
- Biotin deficiency is uncommon since it is synthesised by the intestinal microflora and its ubiquitous occurrence in nature. However, prolonged use of antibiotics that kill the gut bacteria and excess consumption of raw eggs result in biotin deficiency.
- Destruction of gut flora due to prolonged antibiotic use
- High consumption of raw eggs (20 eggs per day)
- Symptoms –
- Anemia, loss of appetite, vomiting, dermatitis, glossitis
- Depression, hallucinations, muscle pains.
Pantothenic Acid
Dietary sources:
- Pantothenate is widely distributed in plants and animals. Excellent food sources include egg yolk, liver, yeast, legumes, whole grains and vegetables.
Daily requirement (RDA): 5-10 mg /day for adults
Functions:
- Mediated through Coenzyme A.
- Involved in all metabolisms
- Hence plays an important role in integrating all the metabolic pathways
- Serves as a carrier of activated acetyl or acyl groups.
- Pyruvate → Acetyl CoA
- α keto glutarate → Succinyl CoA.
- Fatty acid → acyl CoA
Fig: Functions of CoA
Deficiency manifestations:
- Not reported in humans.
- Gopalan – Burning feet syndrome
- Pain & numbness in the toes, sleeplessness & fatigue.
Vitamin B12– (Cyano) Cobalamin
- Anti pernicious anemia vitamin
Co enzymes –
- 5 deoxyadenosyl Cobalamin,
- methylcobalamin
Dietary sources:
- Vitamin B12 is also synthesised by bacteria in colon. It is not found in foods of plant origin. Hence, strict vegans who do not consume milk products are at risk of developing B12 Liver, meat, fish, eggs, milk, curd and cheese are good sources of vitamin B12.
Daily requirement (RDA):
- Adults: 3 micrograms/day
- Children: 0.5- 1.5μg/day
Absorption:
- Dietary source – extrinsic factor of castle
- The stomach secretes Intrinsic factor (IF) from the Parietal cells. This IF combines with vitamin B12.
- The complex then binds to the mucosal cells of Ileum & Thus enters the circulation where it is bound to Transcobalamins I & II.
Image : Absorption, transport & Storage of Vitamin B12.
Functions:
- Red blood cell formation (DNA synthesis).
- Nervous system – maintains myelin sheath around nerves
- Isomerization of Methylmalonyl CoA to Succinyl CoA.
- Synthesis of Methionine from Homocystine.
Deficiency manifestations:
- Megaloblastic anemia
- Subacute combined degeneration
- Demyelination
Pernicious Anaemia:
- Autoimmune destruction of parietal cells that secrete intrinsic factor.
- Low haemoglobin level, decreased number of erythrocytes & neurological symptoms.
- Also associated with neuronal degeneration & demyelination of nervous system.
- Reason for this is that biosynthesis of fatty acids required for myelin formation is impaired, because methylmalonyl CoA acts as competitive inhibitor of malonyl CoA in fatty acid synthesis.
Folic acid
- Active form – tetrahydrofolate(THF)
Dietary sources:
- Folic acid is widely distributed in natural foods. Green leafy vegetables, cereals, fruits, eggs and dairy products are rich sources of folic acid. Bananas, oranges, cauliflower and broccoli contain high levels of folate.
Daily requirement (RDA):
- The RDA of folic acid in adults is about 200 μg/day. During pregnancy (400 μg) and lactation (300 μg).
Functions:
- Important for one carbon metabolism
- THF serves as an acceptor or donor of one carbon units (Formyl, methyl etc.) in amino acid & nucleotide metabolism.
- One carbon unit binds with THF at position N5 or N10.
- The attachment of formyl at position 5 gives N5-formyl THF (Folinic acid/Citrovorum factor)
- N-formylmethionine : Initiator of protein biosynthesis is formed.
- Synthesis of purines(incorporated into DNA)
- Pyrimidine nucleotide –deoxythymidylic acid dTMP(involved in synthesis of DNA)
- Synthesis of glycine, serine, choline, ethanolamine
Deficiency manifestations:
- Most common vitamin deficiency in pregnancy.
- May occur due to reduced dietary intake, defective absorption, use of anticonvulsants & increased demand.
- Macrocytic anemia (Block in DNA synthesis – impairment in maturation of RBCs)
- In pregnant women: Neural tube defects in fetus.
- Hyperhomocysteinemia: Increased risk of atherosclerosis, thrombosis & Hypertension.
Folic acid antagonists:
- Aminopterin & amethopterin (methotrexate): Anticancer drugs
- Trimethoprim (component of septran), pyrimethamine (antimalarial)
- Competitively inhibit dihydrofolate reductase & block the formation of THF.
- Sulfonamides: Structural analogues of PABA
Folate trap or Methyl trap:
- The deficiency of either Folate or vitamin B12 results in similar type of anemia.
- Only 1 metabolic reaction common to folate & vitamin B12.
- The activity of the enzyme homocysteine methyltransferase (Methionine synthase) is low in B12 deficiency.
- As a result the only major pathway for the conversion of N5- methyl THF to THF is blocked & the body THF pool is ↓ed.
- Tissue folate levels are adequate: functional folate deficiency.
- All the folate in the body is trapped as methyl THF. (Folate trap)
- The outcome is Megaloblastic anemia.
- Administration of Methionine has been shown to correct B12 deficiency.
Image : Synthesis of Methionine from Homocysteine – Vitanin B12- Folate trap